Shocking Global Data
▶ Over 300 million women worldwide seek medical attention for reproductive tract infections annually (WHO 2023 Report)
▶ 52% of vaginitis patients are misdiagnosed or inadequately treated (The Lancet Global Multicenter Study, n=45,632)
▶ Mixed infection rates have surged to 34.7%! Among them:
l 18.9% are co-infected with Gardnerella and Candida
l 9.3% have dual infections of Trichomonas and Gardnerella
l 6.5% suffer from a “triple blow” (New England Journal of Medicine 2024)
Clinical Lessons Learned:
“Why does it keep recurring even after a routine vaginal discharge test?”
——Because over 68% of mixed infections are missed by single testing!
Why Must We Use Triple Testing?
➤ Symptoms Are “Copy-Paste”:
Itching/cottage cheese-like discharge ≠ Candida! Trichomonas infections can also mimic “yeast infections.”
Symptoms highly overlap: itching, odor, abnormal discharge, etc., are difficult to distinguish visually.
➤ Missed Detection = Hidden Danger:
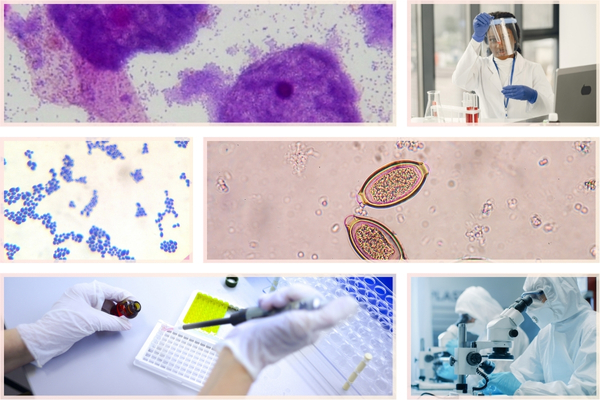
Traditional microscopy miss rates:
Trichomonas: 61%
Gardnerella: 54%
Candida: 39% (JAMA Obstetrics & Gynecology 2023)
Triple testing reduces miss rates by 83%: sensitivity reaches 98.7%.
➤ Mixed Infections Are Surging:
National multicenter studies show that among women aged 30-45, 1 in 5 vaginitis patients is co-infected with ≥2 pathogens.
➤ Wrong Treatment = Antibiotic Resistance Crisis:
Avoid antibiotic misuse: precise diagnosis can reduce unnecessary broad-spectrum antibiotic use by 50%.
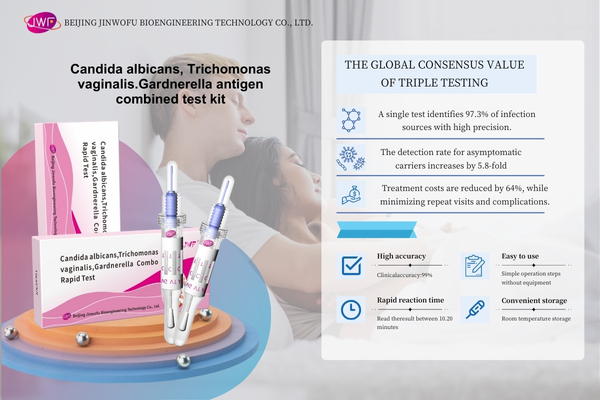
Global Consensus on Triple Testing:
1 test identifies 97.3% of infection sources
1 sample = 3 screenings
Asymptomatic carrier detection rate increases by 5.8 times
Treatment costs reduced by 64%, decreasing repeated visits and complications
Prevents cross-infection (untreated Trichomonas doubles HPV infection risk!)
High-Risk Groups List (Latest FIGO Guidelines)
1. Symptomatic Women
▶ Vulvar itching/burning
▶ Abnormal discharge (cottage cheese-like/yellow-green/foamy)
▶ Pain or bleeding during intercourse
Testing cycle: Test immediately upon symptom onset, retest 7-10 days post-treatment.
2. Asymptomatic but Requiring Screening
▶ Women planning pregnancy (must test within 3 months before conception)
▶ Pregnant women (once each in early, mid, and late pregnancy)
▶ Perimenopausal women (every 6 months)
Data warning: 15% of preterm births are linked to untreated vaginal infections (The Lancet 2023).
3. Sexually Active Women
▶ After a new sexual partner (test within 3 months)
▶ After unprotected sex (test within 72 hours)
▶ If a sexual partner has an infection history (both partners should test simultaneously)
International consensus: 72% of Trichomonas-infected individuals have positive partners (WHO 2024).
4. Immunocompromised Individuals
▶ Diabetics (test every 3 months)
▶ HIV patients (test every 2 months)
▶ Long-term use of immunosuppressants
Research confirms: Diabetics have a 4.3 times higher risk of Candida infection (Diabetes Care Journal).
5. Iatrogenic Exposure
▶ Before intrauterine procedures (abortion/IUD removal/hysterosalpingography, etc.)
▶ Long-term use of broad-spectrum antibiotics
▶ History of vaginal douching
Clinical warning: Improper procedures increase BV infection rates by 89% (US CDC).
6. Recurrent Sufferers
▶ ≥4 episodes annually
▶ Ineffective conventional treatment
▶ Unexplained infertility
Breakthrough discovery: 85% of “recurrences” are actually missed mixed infections (FIGO 2024).
Testing Cycle Summary Table:
Expert Reminder:
“Even without symptoms, annual triple testing is a ‘must’ for women’s health!”
——Chair of the International Vaginal Microecology Alliance (IVMA)
(Note: Data in this article is compiled from WHO, NEJM, JAMA, and other international authoritative reports, with policy updates as of July 2024.)
Post time: Feb-27-2025